Helicobacter pylori (H. pylori) is a gram-negative, spiral-shaped bacterium that primarily inhabits the human stomach. Discovered in 1982 by Australian scientists Barry Marshall and Robin Warren, this bacterium has been identified as the leading cause of many gastrointestinal diseases, including peptic ulcers, chronic gastritis, and even gastric cancer. Before its discovery, the prevailing belief was that stomach ulcers were primarily caused by stress, spicy food, or excessive stomach acid. The identification of H. pylori revolutionized our understanding of gastric diseases, highlighting the role of bacterial infection in their pathogenesis.
Morphology and Physiology
H. pylori is approximately 3 micrometers long and 0.5 micrometers wide, with a distinctive helical shape that aids its movement through the stomach's mucus lining. It possesses several flagella (typically four to six) at one end, allowing it to burrow into the stomach’s mucosal layer. This bacterium is microaerophilic, requiring low oxygen levels to survive, and it is urease-positive, a characteristic that is crucial for its survival in the acidic environment of the stomach.
How Do We Acquire Helicobacter pylori?
H. pylori infection is typically acquired during childhood and can persist throughout life if left untreated. The exact mode of transmission is not fully understood, but it is believed to occur through several possible routes, including fecal-oral, oral-oral, and gastro-oral pathways.
Transmission Routes
- Fecal-Oral Transmission: This is considered the most common mode of transmission. Poor hygiene practices, such as inadequate handwashing after using the bathroom, can lead to contamination of food or water with H. pylori. Consumption of contaminated food or water can then result in infection.
- Oral-Oral Transmission: There is evidence to suggest that H. pylori can be transmitted via saliva. This can occur through kissing or sharing eating utensils, especially in families where close contact is common.
- Gastro-Oral Transmission: This route of transmission involves the regurgitation of stomach contents into the mouth, which can then be transmitted to others. This can happen in scenarios such as vomiting or gastroesophageal reflux.
Risk Factors
Several factors increase the risk of acquiring H. pylori infection:
- Poor Hygiene Conditions: Living in crowded or unsanitary conditions increases the risk of H. pylori transmission.
- Consumption of Contaminated Water: Drinking water contaminated with H. pylori can lead to infection.
- Low Socioeconomic Status: H. pylori infection is more common in populations with lower socioeconomic status, likely due to poorer living conditions and limited access to healthcare.
- Family Members Infected with H. pylori: Close contact with infected individuals, especially family members, increases the likelihood of transmission.
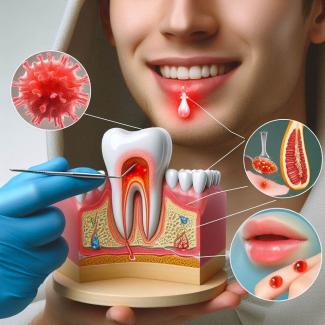
Pathogenesis and Virulence of Helicobacter pylori
The pathogenicity of H. pylori lies in its ability to produce various virulence factors that allow it to survive in the hostile environment of the stomach and cause damage to the host tissues.
Key Virulence Factors
- Urease: H. pylori produces large amounts of urease, an enzyme that catalyzes the conversion of urea into ammonia and carbon dioxide. This reaction helps neutralize the stomach's acidic environment, creating a more favorable condition for the bacterium to thrive.
- CagA (Cytotoxin-Associated Gene A): This protein is associated with more severe disease forms. CagA-positive strains of H. pylori are more likely to cause inflammation, ulcers, and gastric cancer. The CagA protein can disrupt cellular signaling pathways, leading to increased cell proliferation and a higher risk of malignancy.
- VacA (Vacuolating Cytotoxin A): VacA is another toxin that causes the formation of vacuoles in host cells, leading to cell damage and apoptosis. This toxin also interferes with immune responses, allowing the bacterium to survive in the host.
- Adhesins: H. pylori expresses various adhesins that enable it to attach to the epithelial cells of the stomach. This attachment is crucial for colonization and survival in the stomach.
- LPS (Lipopolysaccharides): The LPS on the outer membrane of H. pylori has low immunogenicity, helping the bacterium evade the host's immune system.
How Do We Treat Helicobacter pylori?
The treatment of H. pylori infection typically involves a combination of antibiotics and acid-suppressing medications. The primary goals of treatment are to eradicate the bacterium, heal any associated ulcers, and prevent complications such as gastric cancer.
Standard Triple Therapy
For many years, the standard treatment for H. pylori infection has been triple therapy, which includes:
- Proton Pump Inhibitor (PPI): Medications such as omeprazole, lansoprazole, or esomeprazole are used to reduce stomach acid production. Lowering stomach acidity enhances the effectiveness of antibiotics and promotes ulcer healing.
- Clarithromycin: This macrolide antibiotic is commonly used in combination therapy due to its effectiveness against H. pylori.
- Amoxicillin or Metronidazole: Amoxicillin is a penicillin antibiotic, while metronidazole is a nitroimidazole antibiotic. Either of these can be used alongside clarithromycin to complete the triple therapy regimen.
The usual duration of triple therapy is 10 to 14 days. However, the emergence of antibiotic resistance, particularly to clarithromycin, has led to a decrease in the success rates of this regimen.
Sequential Therapy
Sequential therapy is a variation of standard triple therapy. It involves administering a PPI and amoxicillin for the first five days, followed by a PPI, clarithromycin, and metronidazole for the next five days. This approach reduces the likelihood of antibiotic resistance by using different drug combinations at different times.
Quadruple Therapy
Quadruple therapy is often used in regions with high rates of clarithromycin resistance or in cases where initial therapy has failed. This regimen typically includes:
- PPI: To reduce stomach acid.
- Bismuth Subsalicylate: A compound that coats ulcers and protects them from stomach acid, also possessing some antibacterial activity against H. pylori.
- Tetracycline: An antibiotic effective against H. pylori.
- Metronidazole: Another antibiotic used to eradicate the bacterium.
Quadruple therapy is usually administered for 10 to 14 days and has shown higher eradication rates compared to standard triple therapy.
Levofloxacin-Based Therapy
In cases of multiple treatment failures or confirmed resistance to multiple antibiotics, doctors may prescribe a regimen based on levofloxacin, a quinolone antibiotic. This regimen typically includes:
- Levofloxacin: An antibiotic used to combat bacteria resistant to other antibiotics.
- Amoxicillin: Included to provide a broader spectrum of action.
- PPI: To reduce stomach acidity and increase the effectiveness of antibiotics.
Levofloxacin-based therapy can be effective, but care must be taken to monitor for the development of resistance, so this approach is mainly used when other therapies have failed.
What Tests Are Available for Helicobacter pylori?
Several diagnostic tests are available to detect H. pylori infection. These tests can be categorized into invasive and non-invasive methods.
Invasive Tests
- Endoscopy with Biopsy: This is the most direct method for diagnosing H. pylori infection. During an endoscopy, a thin, flexible tube with a camera (endoscope) is passed through the mouth into the stomach. A gastroenterologist can visually examine the stomach lining and take biopsies (small tissue samples) from the stomach and duodenum. These biopsies are then tested for the presence of H. pylori using methods such as histology, rapid urease test, or culture.
- Histology: Biopsy samples are stained and examined under a microscope to check for the presence of H. pylori. This method is highly accurate and can also provide information about the extent of inflammation or damage to the stomach lining.
- Rapid Urease Test: This test involves placing a biopsy sample in a medium containing urea and a pH indicator. If H. pylori is present, its urease activity will convert urea into ammonia, raising the pH and causing a color change in the medium.
- Culture: Although not commonly performed due to its complexity, culturing H. pylori from a biopsy allows for antibiotic susceptibility testing, which can be useful in cases of antibiotic resistance.
Non-Invasive Tests
- Urea Breath Test: This is one of the most widely used non-invasive tests for H. pylori. The patient ingests a substance containing urea labeled with a carbon isotope (C-13 or C-14). If H. pylori is present in the stomach, its urease enzyme will break down the urea, releasing labeled carbon dioxide, which is then exhaled and measured. This test is highly sensitive and specific and is often used to diagnose H. pylori infection and confirm eradication after treatment.
- Serological Tests: Blood tests can detect antibodies against H. pylori. However, these tests cannot differentiate between active and past infections, as antibodies may persist in the blood long after the infection has been eradicated. Therefore, serology is less commonly used for diagnosing active infection.
- Stool Antigen Test: This test detects the presence of H. pylori antigens in a stool sample. It is a non-invasive, accurate, and convenient method for diagnosing H. pylori infection and confirming eradication after treatment.
- Molecular Tests: Polymerase chain reaction (PCR) can detect H. pylori DNA in biopsy, stool, or gastric juice samples. This method is highly sensitive and can also detect specific genetic markers associated with antibiotic resistance.
Symptoms and Consequences of Helicobacter pylori Infection
Chronic Gastritis
Chronic gastritis is long-term inflammation of the stomach lining, often caused by H. pylori. The infection can cause diffuse inflammation affecting the entire stomach lining or more localized inflammation affecting primarily the antrum of the stomach. Symptoms of chronic gastritis include upper abdominal pain, nausea, loss of appetite, and bloating.
Peptic Ulcers
H. pylori is the main cause of most peptic ulcers that develop in the stomach or duodenum. The bacterium damages the protective mucus lining of the stomach, allowing stomach acid to come into contact with sensitive tissues, leading to the formation of ulcers. Symptoms include burning stomach pain, usually occurring between meals or at night, nausea, vomiting, and weight loss.
Stomach Cancer
Long-term infection with H. pylori can lead to stomach cancer, particularly adenocarcinoma. The carcinogenesis process involves a sequence of changes triggered by chronic inflammation, atrophic gastritis, intestinal metaplasia, and dysplasia, leading to the development of cancer. Infection with CagA-positive strains of H. pylori is particularly associated with an increased risk of developing stomach cancer.
MALT Lymphoma
H. pylori is also associated with the development of MALT lymphoma (mucosa-associated lymphoid tissue), a rare type of stomach cancer originating from lymphoid tissue associated with the mucosa. Early stages of MALT lymphoma are often linked to H. pylori infection, and in many cases, eradication of the bacterium can lead to remission of the lymphoma.
Prevention of Helicobacter pylori Infection
Currently, no vaccine is available against H. pylori, so preventive measures focus on improving hygiene practices and living conditions.
Improving Hygiene Practices
- Hand Washing: Regular and thorough hand washing with soap, especially after using the bathroom and before eating, is crucial for preventing H. pylori infection.
- Safe Food Preparation: Ensuring that food is thoroughly cooked and that strict hygiene standards are followed during preparation can reduce the risk of infection.
- Safe Drinking Water: Using purified or boiled water for drinking, especially in regions with poor sanitation, is an important preventive measure.
Public Awareness
- Education: Public education about the modes of transmission of H. pylori and the importance of hygiene practices is essential for reducing the incidence of infections.
- Early Detection and Treatment: Identifying and treating H. pylori infection in patients with peptic ulcers or gastritis can prevent more serious complications, such as stomach cancer or MALT lymphoma.
H. pylori infection is a global health issue affecting more than half of the world's population. Understanding the nature of this bacterium, its modes of transmission, pathogenicity, and methods for detection and treatment is crucial for managing diseases associated with H. pylori. Advances in diagnostics and treatment have made it possible to effectively eradicate this bacterium, but antibiotic resistance and reinfection remain challenges that require further research and improvements in preventive strategies.