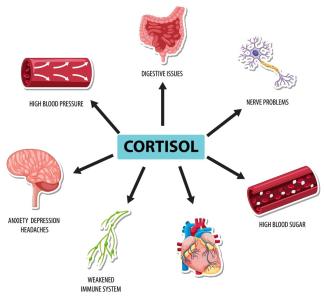
Cortisol is a critical hormone produced by the adrenal glands, located just above the kidneys. It plays an essential role in the body's response to stress and helps regulate several vital physiological functions, including metabolism, immune response, inflammation control, and maintaining blood pressure. Cortisol also assists in maintaining blood sugar levels, balances salt and water in the body, and helps manage energy levels during stressful events.
A typical daily cortisol rhythm is highest in the morning, around 6 to 8 AM, and lowest at night. Dysregulation in cortisol production, whether too high or too low, can have significant health consequences. Low cortisol, or hypocortisolism, presents unique challenges and potential risks that need to be carefully understood and managed.
What Does Low Cortisol Mean?
Low cortisol, medically termed adrenal insufficiency or hypocortisolism, occurs when the adrenal glands do not produce enough cortisol. There are two primary forms of adrenal insufficiency:
- Primary adrenal insufficiency (Addison's disease): This occurs when the adrenal glands are directly damaged and unable to produce cortisol. Most commonly, this damage is due to autoimmune disease, where the body’s immune system attacks the adrenal glands. Other causes include infections like tuberculosis, cancer metastasis, or genetic conditions affecting the adrenal glands.
- Secondary adrenal insufficiency: This results from insufficient stimulation of the adrenal glands by adrenocorticotropic hormone (ACTH), a hormone produced by the pituitary gland. In this case, the adrenal glands themselves are not defective, but they are not receiving adequate signals to produce cortisol. Common causes include damage to the pituitary gland from tumors, surgeries, or long-term steroid use.
In both cases, the body’s ability to handle stress—whether physical, emotional, or metabolic—is compromised.
Is Low Cortisol Dangerous to Health?
Yes, low cortisol levels can be dangerous, especially if left untreated. Cortisol plays a pivotal role in managing the body's response to stress. Without sufficient cortisol, the body cannot mount an adequate response to physical stressors like illness or injury, which can result in serious complications. One of the most dangerous consequences of low cortisol is an adrenal crisis, a potentially life-threatening condition.
Adrenal Crisis
In severe cases, low cortisol can lead to an adrenal crisis, which is a medical emergency characterized by:
- Sudden, severe pain in the lower back, abdomen, or legs
- Severe vomiting and diarrhea
- Low blood pressure and shock
- Confusion, loss of consciousness, or coma
Without prompt treatment, adrenal crisis can be fatal, as the body's vital functions, including blood pressure regulation, collapse.
Other chronic complications of untreated low cortisol include:
- Hypoglycemia (low blood sugar)
- Hyponatremia (low sodium levels in the blood)
- Chronic fatigue and weakness
- Impaired immune function
What Are the Symptoms of Low Cortisol?
The symptoms of low cortisol can develop gradually and be mistaken for other conditions, which can make diagnosis difficult. Common symptoms of adrenal insufficiency include:
- Chronic Fatigue: People with low cortisol often feel persistently tired, even after rest. This fatigue can be debilitating and worsen with physical or emotional stress.
- Weight Loss and Appetite Reduction: Unexplained weight loss is common as cortisol plays a role in regulating metabolism and appetite. Loss of appetite often accompanies this.
- Muscle Weakness: Weakness, particularly in the muscles, is another common symptom. Cortisol supports muscle function by maintaining glucose availability during physical activity, and its deficiency can lead to weakness.
- Low Blood Pressure: Cortisol helps maintain blood pressure by supporting vascular tone. People with low cortisol often experience low blood pressure, dizziness, or even fainting, especially when standing up (orthostatic hypotension).
- Low Blood Sugar (Hypoglycemia): Cortisol is vital for maintaining blood glucose levels between meals. Hypoglycemia can cause shakiness, sweating, confusion, and severe fatigue.
- Darkening of the Skin: In cases of primary adrenal insufficiency, a person may develop hyperpigmentation, especially in areas of friction like elbows, knees, and scars. This occurs due to increased ACTH levels, which stimulates melanin production in the skin.
- Mood Disturbances: Depression, irritability, and anxiety are common symptoms due to the effects of cortisol deficiency on brain function and mood regulation.
Can I Do a Cortisol Test at Home?
Yes, it is possible to measure cortisol levels at home using saliva or urine-based tests. These home tests can give you an idea of your cortisol levels, especially if conducted at specific times of the day, such as in the morning or evening, when cortisol levels are expected to vary naturally.
However, home cortisol tests should not be seen as a replacement for professional medical evaluation. They can provide some initial insight, but interpretation of results and further testing should be done under the guidance of a healthcare provider.
How Do We Do a Home Cortisol Test?
There are two primary methods of measuring cortisol at home:
- Saliva Test: This involves collecting a small amount of saliva using a provided collection kit. Saliva samples are usually taken multiple times a day (e.g., morning, noon, evening) to capture the diurnal rhythm of cortisol secretion. Once the samples are collected, they are sent to a laboratory for analysis.
- Urine Test: A 24-hour urine cortisol test can be done at home by collecting all the urine passed in a 24-hour period. This test measures free cortisol, which is the unbound, biologically active form of cortisol.
Both tests are easy to use but require proper collection and shipping to ensure accurate results. Always follow the instructions provided with the test kit to avoid contamination or inaccurate readings.
Blood Test for Free Cortisol and ACTH Test
Blood Test for Free Cortisol
A blood test for free cortisol is a direct method for assessing cortisol levels in the bloodstream. This test is typically done in the morning when cortisol levels are at their peak. It can provide valuable information about adrenal gland function, but a single cortisol measurement is usually not enough to diagnose adrenal insufficiency. Instead, it is often part of a broader set of tests.
ACTH Stimulation Test (Cortisol Load Test)
The ACTH stimulation test is a more definitive diagnostic tool for evaluating adrenal insufficiency. It involves injecting synthetic ACTH into the bloodstream and measuring the adrenal glands’ response in terms of cortisol production.
- Procedure: The patient’s baseline cortisol level is first measured. Then, synthetic ACTH is injected, and cortisol levels are measured again after 30 and 60 minutes.
- Interpretation: If cortisol levels rise appropriately after the injection, it suggests the adrenal glands are functioning normally, and the problem may lie with the pituitary gland (secondary adrenal insufficiency). If cortisol levels do not rise sufficiently, it indicates primary adrenal insufficiency (Addison's disease).
This test is considered the gold standard for diagnosing adrenal insufficiency and should be performed in a medical setting under the supervision of a healthcare professional.
Treating Low Cortisol
Treatment for low cortisol depends on the underlying cause and typically involves hormone replacement therapy to restore normal cortisol levels. The most common treatments include:
- Glucocorticoid Replacement: This involves taking medications like hydrocortisone, prednisone, or dexamethasone to replace the missing cortisol. These drugs help regulate metabolism, reduce inflammation, and maintain blood pressure.
- Mineralocorticoid Replacement: For those with Addison’s disease, fludrocortisone may be prescribed to replace aldosterone, another hormone produced by the adrenal glands that regulates salt and water balance.
- Managing Stress: Since people with adrenal insufficiency have difficulty handling physical and emotional stress, it is essential to adjust medication during periods of illness, surgery, or severe stress. This may include increasing the dose of glucocorticoids temporarily to prevent adrenal crisis.
- Education and Crisis Management: Patients with low cortisol must be educated on how to manage their condition, recognize signs of adrenal crisis, and know when to seek emergency treatment. Wearing a medical alert bracelet and carrying an emergency injection of hydrocortisone is often recommended for patients at risk of adrenal crisis.
Low cortisol is a serious condition that can lead to significant health problems if left untreated. While home tests can provide useful insights, definitive diagnosis and management should always be done under the guidance of a healthcare professional. Treatment typically involves hormone replacement therapy to restore normal cortisol levels and prevent complications such as adrenal crisis.