Migraine headaches are a type of headache that can cause severe throbbing or pulsing pain, often on one side of the head. They are often accompanied by other symptoms, including nausea and sometimes vomiting. This combination of symptoms is sometimes referred to as "migraine with nausea."
Here are some key points about migraines and nausea:
- Nausea and Vomiting: Nausea is a common symptom of migraines, and some people with migraines also experience vomiting. This nausea can be quite severe and can make the overall migraine experience even more distressing.
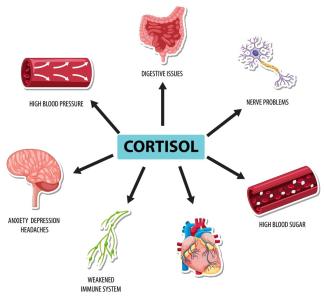
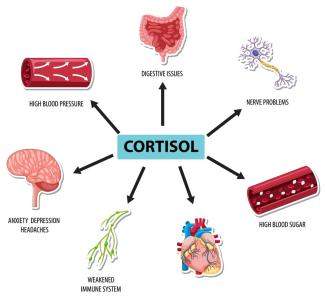
- Migraine Triggers: Migraine triggers can vary from person to person but may include stress, certain foods, hormonal changes, lack of sleep, weather changes, and more. Identifying and avoiding triggers can help reduce the frequency and severity of migraine attacks.
- Aura: Some people with migraines experience an "aura" before the headache phase. Auras are typically visual disturbances but can also involve other sensory symptoms. Nausea can sometimes occur during the aura phase or shortly before the headache phase.
- Medications: There are various medications available to treat migraines, including those that specifically target nausea and vomiting. These can help alleviate these symptoms during a migraine attack.
- Lifestyle Management: Along with medications, lifestyle modifications can be helpful in managing migraines. These may include maintaining a regular sleep schedule, staying hydrated, managing stress, and avoiding triggers.
- Consult a Healthcare Provider: If you experience severe or frequent migraines with nausea, it's essential to consult a healthcare provider. They can help diagnose your condition, develop a treatment plan, and prescribe appropriate medications if necessary.
- Emergency Situations: In some cases, a migraine can be so severe that it requires emergency medical attention. If you experience a sudden and severe headache, confusion, difficulty speaking, weakness or numbness on one side of the body, or other unusual symptoms during a headache, seek immediate medical help, as these could be signs of a more serious condition, such as a migraine variant or stroke.
It's important to work with a healthcare provider to manage your migraines effectively. They can help you find the most appropriate treatment options to alleviate your symptoms and improve your quality of life.
Symptoms migraine
Migraine symptoms can vary from person to person and can also differ in terms of severity and duration. Migraines typically progress through stages, although not everyone experiences all of these stages. The common symptoms of a migraine include:
- Prodrome (pre-headache phase):
- Mood changes (e.g., irritability, depression).
- Food cravings.
- Increased thirst and urination.
- Fatigue and yawning.
- Neck stiffness.
- Visual disturbances (e.g., seeing flashing lights or blind spots, known as auras, though auras can also occur during the headache phase).
- Aura (not everyone experiences this):
- Visual disturbances (e.g., zigzag lines, shimmering spots).
- Sensory changes (e.g., tingling or numbness in the face or extremities).
- Speech difficulties.
- Headache phase:
- Throbbing or pulsating pain, often on one side of the head.
- Intense and severe headache.
- Sensitivity to light (photophobia).
- Sensitivity to sound (phonophobia).
- Nausea.
- Vomiting.
- Dizziness.
- Blurred vision.
- Postdrome (post-headache phase):
- Fatigue.
- Confusion.
- Mood changes (e.g., feeling "hungover" or elated).
- Muscle aches and weakness.
- Scalp tenderness.
The duration of each phase can vary. Some migraines may last for a few hours, while others can persist for several days. It's important to note that not all migraine sufferers experience the aura phase, and some may experience atypical symptoms or symptoms that change from one migraine episode to another.
If you experience severe and recurrent headaches with any of these symptoms, especially if they significantly impact your daily life, it's essential to consult a healthcare provider. They can help diagnose your condition, recommend appropriate treatment options, and provide guidance on managing and preventing migraines. Management may involve lifestyle modifications, prescription medications, and acute treatments for when a migraine attack occurs.
How to treat migraine diagnostic and testing
The diagnosis and treatment of migraines typically involve a combination of medical evaluation, symptom assessment, and, in some cases, testing to rule out other underlying conditions. Here's a general overview of how migraines are diagnosed and treated:
1. Clinical Evaluation:
- Medical History: Your healthcare provider will start by taking a detailed medical history. They will ask about the frequency, duration, and characteristics of your headaches, as well as any associated symptoms.
- Family History: Migraines can have a genetic component, so your family's medical history may be relevant.
- Triggers: Discuss potential migraine triggers such as specific foods, stress, hormonal changes, or environmental factors.
- Other Health Conditions: Mention any other health conditions you have, as some medical conditions can mimic migraine symptoms.
2. Physical Examination:
- A physical exam is typically performed to rule out other medical conditions that could be causing your symptoms.
3. Diagnostic Criteria:
- Your healthcare provider will often use established diagnostic criteria, such as the International Classification of Headache Disorders (ICHD), to determine if your symptoms meet the criteria for migraines.
4. Imaging and Testing (if necessary):
- In most cases, migraines can be diagnosed based on clinical evaluation alone. However, your healthcare provider may order additional tests if they suspect other underlying conditions or if your symptoms are atypical. These tests may include:
- MRI or CT Scan: These imaging tests can help rule out other neurological conditions that may be causing similar symptoms.
- Blood Tests: Blood tests may be done to rule out conditions like infections or metabolic disorders that can cause headaches.
5. Treatment:
- Once a diagnosis of migraines is established, treatment options will be discussed. Migraine treatment typically includes two approaches:
- Acute Treatment: Medications taken during a migraine attack to relieve symptoms. These may include pain relievers (e.g., NSAIDs or prescription migraine medications) and anti-nausea drugs.
- Preventive Treatment: Medications taken regularly to reduce the frequency and severity of migraine attacks. Preventive medications are typically considered if you have frequent or severe migraines that significantly impact your daily life.
6. Lifestyle Modifications:
- Your healthcare provider may recommend lifestyle modifications to help manage migraines. These can include identifying and avoiding triggers, maintaining a regular sleep schedule, managing stress, and adopting a consistent meal routine.
7. Follow-Up:
- It's important to follow up with your healthcare provider regularly to monitor your progress, adjust your treatment plan as needed, and discuss any changes in your symptoms.
Remember that the specific diagnostic and treatment approach may vary from person to person, and it's essential to work closely with your healthcare provider to develop an individualized plan that suits your needs. If you experience severe or unusual symptoms, seek immediate medical attention to rule out other serious conditions.
Migraine medical support team
Managing migraines often involves working with a medical support team to ensure comprehensive care. This team typically includes various healthcare professionals who specialize in different aspects of migraine diagnosis, treatment, and support. Here's an overview of the members of a migraine medical support team:
- Primary Care Physician (PCP): Your primary care physician is often the first point of contact for migraine evaluation and management. They can diagnose migraines, recommend initial treatments, and refer you to specialists if needed.
- Neurologist: Neurologists are medical doctors who specialize in the nervous system, including the brain. They often have expertise in diagnosing and treating migraines and can help manage more complex cases.
- Headache Specialist: Some neurologists or other healthcare providers specialize specifically in headaches and migraines. They are well-versed in the latest migraine treatments and can provide specialized care.
- Pain Management Specialist: In some cases, a pain management specialist may be part of your team, particularly if you have chronic migraine pain that is challenging to control.
- Psychologist or Psychiatrist: Mental health professionals can be valuable members of your team, especially if you have comorbid mental health conditions such as anxiety or depression, which can exacerbate migraines. They can provide counseling and therapy to help you manage stress and improve your coping strategies.
- Pharmacist: Pharmacists play a crucial role in your treatment by helping you understand your medications, potential side effects, and drug interactions. They can also provide guidance on over-the-counter remedies.
- Nutritionist/Dietitian: Dietary factors can trigger migraines in some individuals. A nutritionist or dietitian can help identify trigger foods and develop a diet plan that reduces the likelihood of migraine attacks.
- Physical Therapist: Physical therapists can provide exercises and techniques to improve posture, reduce muscle tension, and relieve neck and shoulder pain, which may contribute to migraines.
- Acupuncturist or Alternative Therapist: Some people find relief from migraines through complementary and alternative therapies like acupuncture, biofeedback, or mindfulness-based stress reduction. These practitioners can be part of your support team if you choose to explore these options.
- Patient Advocate or Support Group: Joining a migraine support group or having access to a patient advocate can provide emotional support, share coping strategies, and help you navigate the healthcare system.
- Health Insurance Specialist: If your insurance coverage is a concern, a specialist can help you understand your policy and assist with obtaining coverage for migraine-related treatments and medications.
Effective communication and collaboration among these healthcare professionals are essential for managing migraines comprehensively. Make sure to keep all members of your medical support team informed about your symptoms, treatments, and any changes in your condition. This coordinated approach can help optimize your migraine management and improve your quality of life.